What is World Keratoconus Day?
World Keratoconus Day is celebrated each year on November 10th. The day is dedicated to raising awareness around keratoconus while educating and advocating for those living with the condition. This World KC Day, we show support by educating patients, friends, and family about keratoconus.
What is Keratoconus?
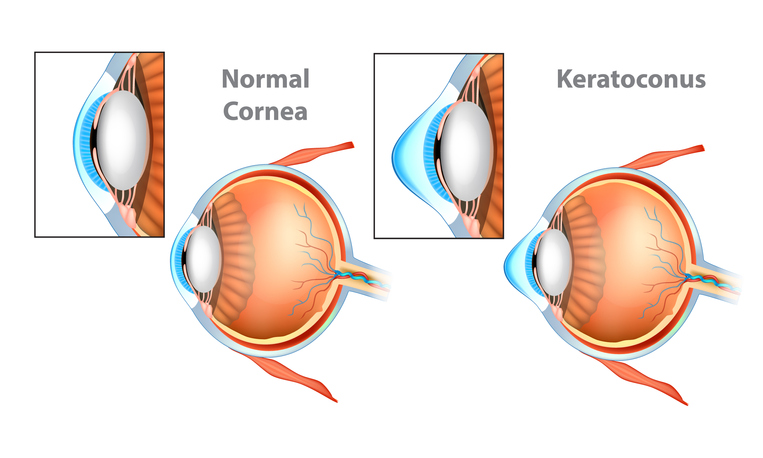
Normal Cornea and Keratoconus (KC) Cornea.
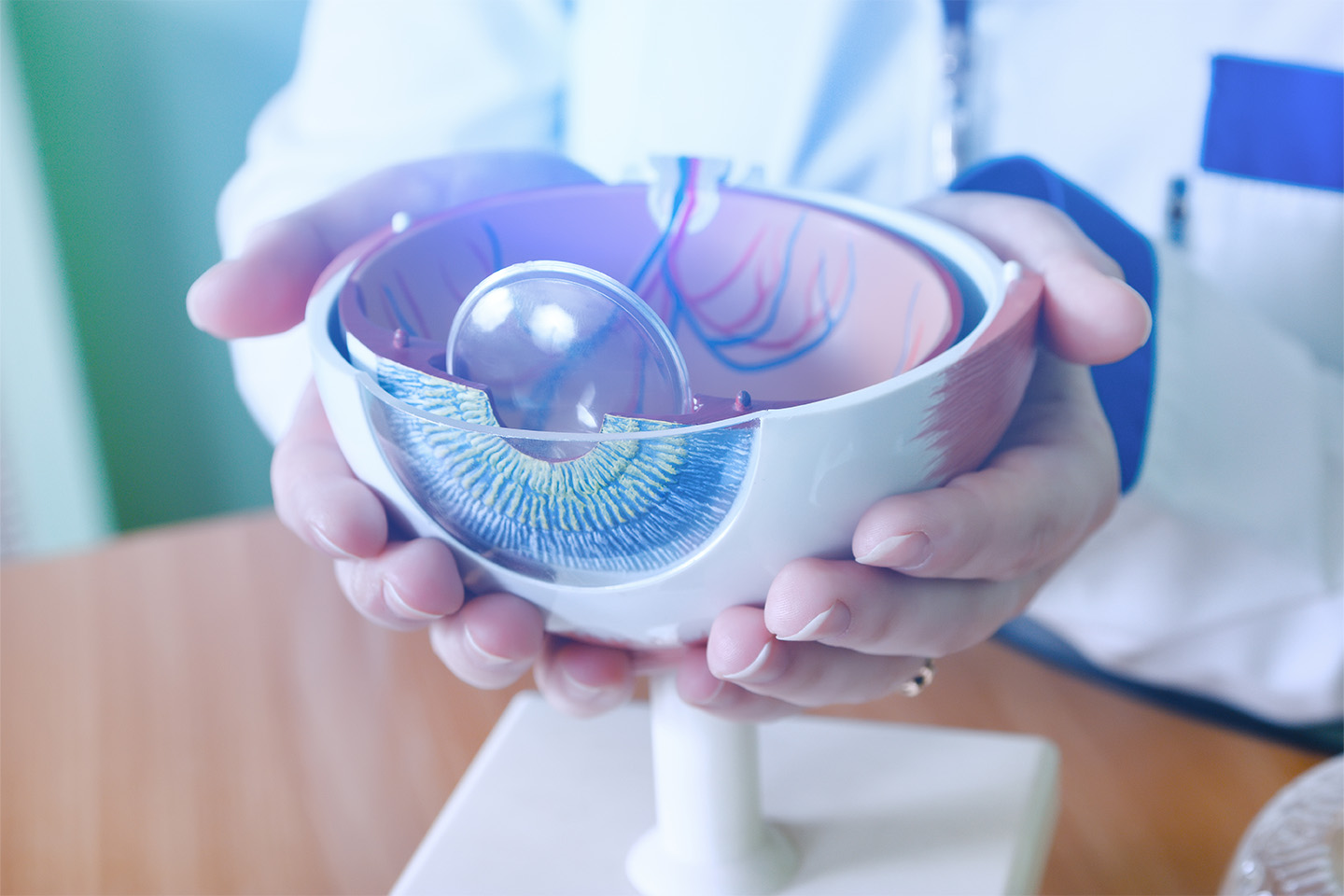
Keratoconus, or KC, is a common eye condition that impacts the cornea, which is the clear, transparent lens that covers the front part of the eye. The cornea becomes thin and develops a cone-like bulge.
Structure of the Cornea:
The cornea is made of collagen fibers, a protein structure that makes the cornea strong and flexible. A healthy cornea has a round, symmetrical shape that collagen helps to maintain. The primary functions of the cornea include preventing foreign matter from entering the interior of the eye and, of primary interest to those with KC, helping to focus the light that enters the eye.
Changes and Symptoms

Keratoconus – eye disease, thinning of the cornea in the form of a cone.
KC occurs when the clear, typically dome-shaped cornea thins and weakens to the point that it gradually bulges outward, shifting into a cone-like shape. An abnormally shaped cornea makes it difficult for the eye to focus light, which can cause blurred or distorted vision, including nearsightedness and irregular astigmatism.
Common symptoms of keratoconus include:
- Blurred or distorted vision
- Sensitivity to light
- Glares or halos around lights
- Difficulty driving at night
- Changing prescriptions
- Eye irritation
- Headaches associated with eye pain
Keratoconus usually occurs in both eyes, but one eye is still quite common.
Potential Causes
While the cause of keratoconus is unknown, genetic and environmental factors contribute.
- Genetics. Although KC does not appear to have a definitive genetic cause, research suggests that around 1 in 10 people with KC also have a parent with the condition; however, different studies report a variety of rates. This may allude to a genetic predisposition towards developing keratoconus, but familial correlation could also stem from similarity in environments.
- Chronic eye inflammation from allergies or other irritants can help encourage destruction of corneal tissue.
- Frequent eye rubbing increases the risk of developing keratoconus and is a risk factor for the progression of the disease.
When Does KC Occur?
Keratoconus usually occurs during the teenage years into the early 20s. Degeneration continues for 10-20 years until the progression gradually slows and stops. The severity when progression stops can range from mild astigmatism to severe thinning.
How Common is Keratoconus?
While keratoconus is a rare disease that affects fewer than 200,000 people in the United States, it is one of the more common corneal conditions. Recent studies in the U.S. have found that this progressive eye condition affects approximately 1 in 2,000 people alone.
Being diagnosed with a rare disease might seem scary; however, finding a community and a physician to start treatment has never been easier. Online resources and networks can be incredibly helpful in understanding diagnosis and treatment options.
Treatment Options for Keratoconus

Treatment of keratoconus depends on the severity of the disease and mainly focuses on correcting vision. While early interventions can help to slow the process, it will not keep keratoconus at bay.
Diagnosis:
The first step in treatment is proper diagnosis. When a patient shows up with symptoms of keratoconus, it is important to take action quickly to combat the condition’s progressive nature. Patients often present with the symptoms listed earlier, prompting the provider to do an in-depth eye exam, which will include measurement of the cornea’s curvature through corneal topography.
Corneal topography creates a computerized map of the curve of the cornea and is integral to following the progression of KC. Additional tests that a doctor might run to confirm diagnosis include a slit-lamp exam, which can help detect abnormalities in the outer and middle layer of the cornea, and pachymetry, which is used to measure the thinnest areas of the cornea.
Early/Mild Stages:
In the early stages of KC, the use of glasses or soft contact lenses to treat nearsightedness or astigmatism might be sufficient to correct vision problems. However, as the keratoconus progresses and glasses can no longer provide sufficiently clear vision, the patient will need to be fitted with a more custom type of contact lens. These may include rigid gas permeable, or RGP lenses, hybrids, or larger lenses such as sclerals.
If the KC progresses, one option for treatment is a minimally invasive outpatient procedure known as corneal cross-linking. The FDA approved corneal-cross linking in 2016 after clinical trials showed that it could stop the bulging of the cornea within 3 months to a year after the procedure. In some cases, it could even produce a mild reversal in the corneal bulging.
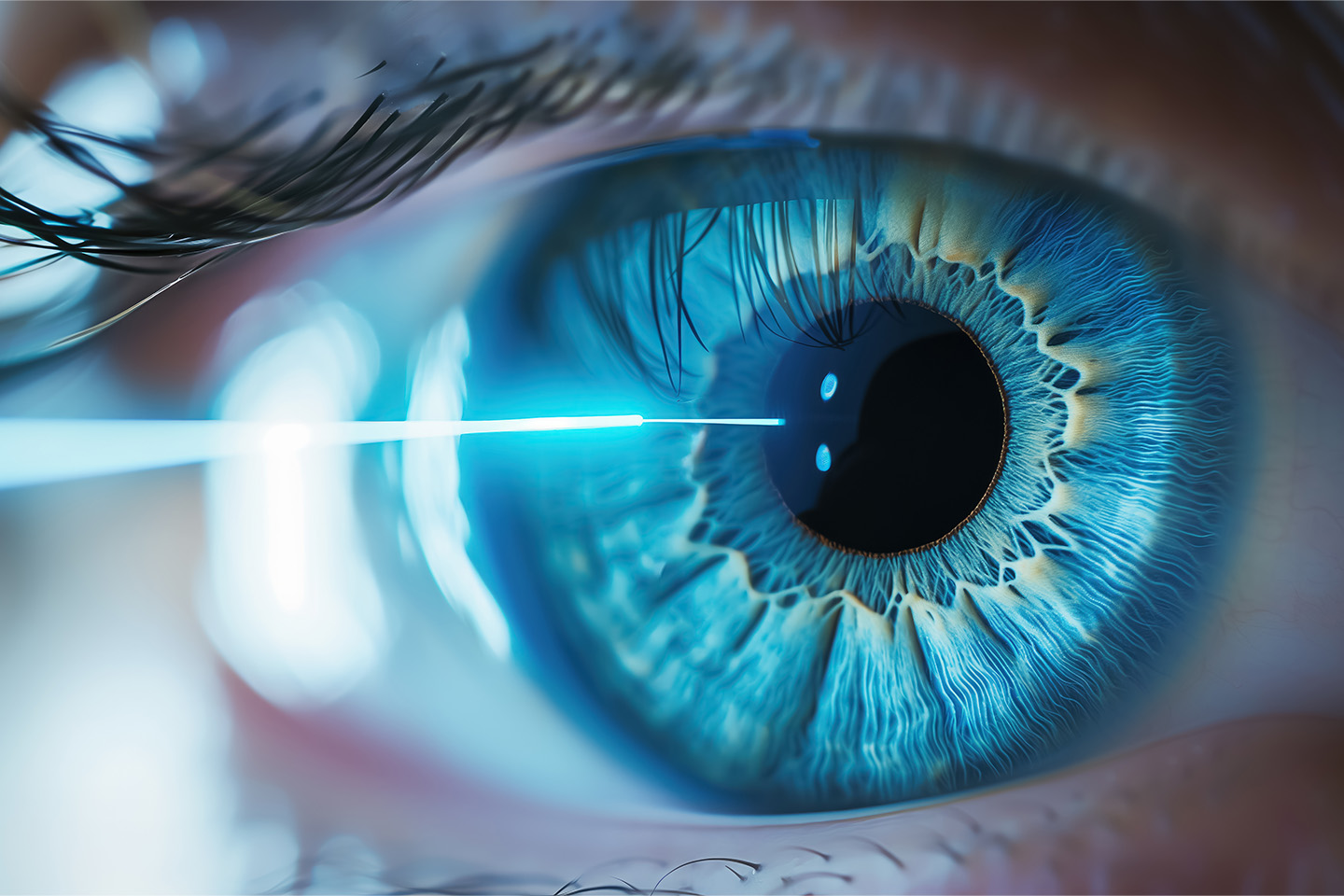
Corneal cross-linking involves the application of Riboflavin, generally administered as eye drops, to the eye. The solution is then activated by UVA light for about 30 minutes. The activation of the solution causes new collagen bonds to form, recovering and preserving the strength and shape of the cornea.
The procedure may require the removal of the thin outer layer of the cornea, known as the corneal epithelium. This will allow greater tissue penetration by the medication, increasing the effectiveness of the cross-linking procedure by strengthening corneal collagen at a deeper level. While it is not possible to completely restore the cornea to its original healthy state, treatment can prevent vision from getting progressively worse or even, in some cases, may improve vision. Stabilizing the cornea as early as possible is crucial to avoid a cornea transplant
Intermediate Stages:
Intermediate keratoconus patients can also undergo corneal cross-linking, but only to a certain extent. If their corneas become too thin, they are no longer a candidate. Crosslinking is ideally performed as early as possible in order to prevent progression of KC. Patients diagnosed with KC that are showing progression after 6-12 months should ideally get cross-linking as soon as possible.
Advanced Stages:
In the more severe cases of keratoconus, treatment options are more invasive and depend on the severity of corneal scarring, the extent of corneal thinning, or continued poor vision with even the strongest of prescription lenses.
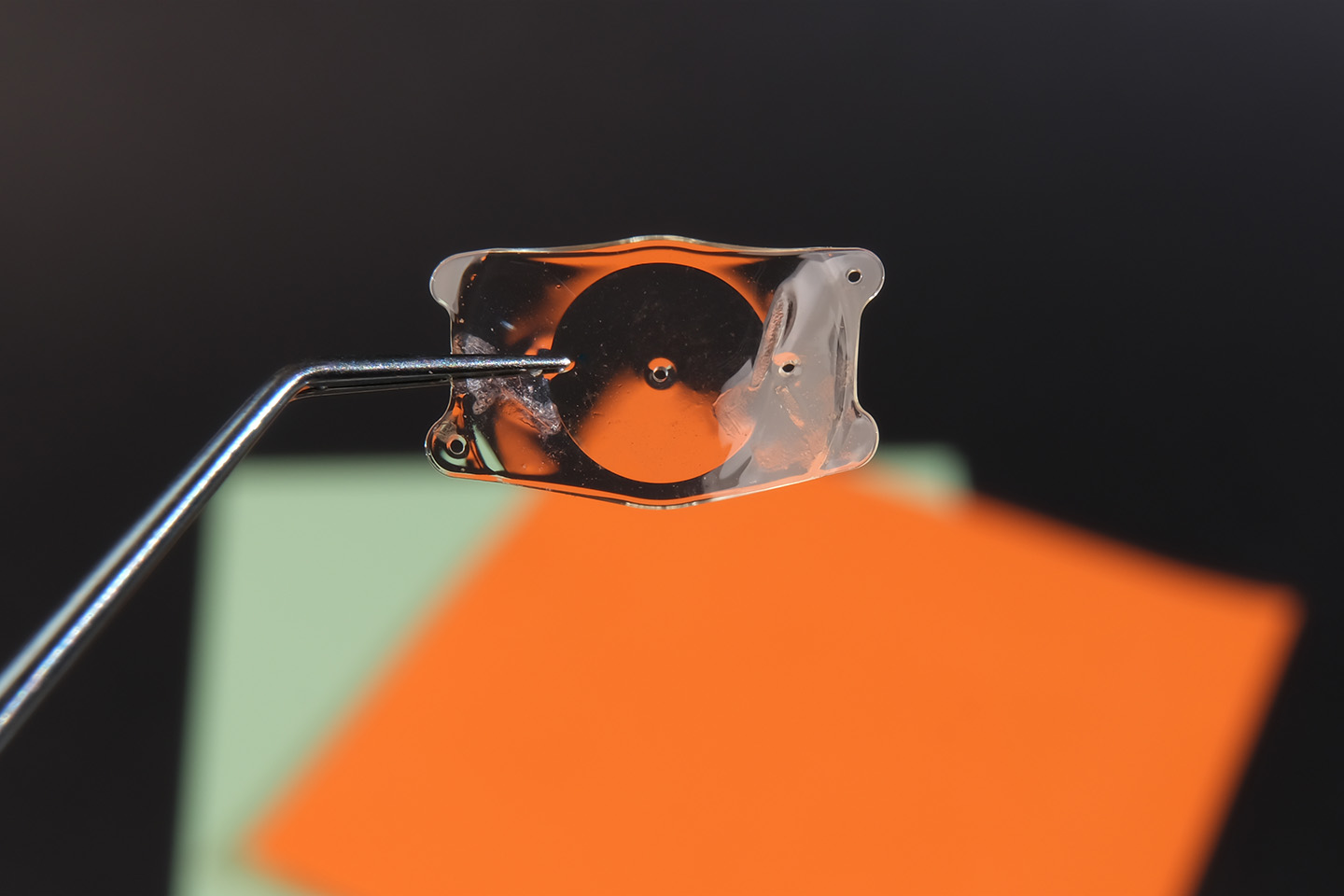
One treatment option is a corneal ring (INTAC), a small plastic ring implanted into the middle layer of the cornea. Standard contacts often become too uncomfortable to wear as the severity of KC increases. These implants, however, can be a perfect solution in their ability to change the cone shape of the affected cornea and flatten it enough so standard contact lenses can fit comfortably.
Another treatment route for severe keratoconus is corneal transplant surgery. Depending on the location of the bulge and the severity of the disease, there are two types of corneal transplant.
- The first type is penetrating keratoplasty, a full-thickness transplant of the cornea. In this procedure, the doctor removes the patient’s cornea and replaces it with donor tissue.
- The second type of transplant is called deep anterior lamellar keratoplasty (DALK). The DALK procedure differs from penetrating keratoplasty as it preserves the corneal endothelium, the most interior layer, and grafts donor tissue on top of it. This method helps to avoid the rejection of tissue in the critical inner lining that can occur with a penetrating keratoplasty.
Corneal transplants are typically performed as outpatient procedures and take about an hour to complete. Potential complications of the surgery include graft rejection, infection, and astigmatism. It is important to note, however, that complications can be expected with any invasive surgical treatment, and corneal transplantation is overall very successful.
Patients should expect their vision to remain blurry for 3 to 6 months following the procedure. Astigmatism post-surgery can often be managed by wearing contact lenses, which is typically more comfortable after the transplant.
Contact Lens Options for Keratoconus
Many types of corrective lenses are available for management of poor vision due to keratoconus. It is important that patients work with providers to decide which option is right for them.
Soft contact lenses are the first choice for early stages of keratoconus, as they can help manage blurry or distorted vision for a time. However, due to the progressive nature of the disease, as the shape of the cornea changes, so will the prescription. Patients may find themselves needing different prescriptions frequently.
- Hard contact lenses, also known as rigid or rigid gas permeable lenses, are the next step in treating the advancement of keratoconus. This type of lens is made to fit each patient’s individual cornea and mimics a smooth optical surface to focus light through, resulting in crisper vision. Hard lenses may feel uncomfortable at first, but many patients adjust well to wearing them. If rigid lenses are uncomfortable, “piggybacking” a hard contact lens on top of a soft one may alleviate some of the discomfort.
- Hybrid lenses are special contact lenses with rigid centers surrounded by a softer ring. This type of lens capitalizes on the visual acuity synonymous with hard lenses while maintaining some of the comfort experienced with soft lenses. Some patients that have difficulty with hard lenses frequently prefer wearing hybrid lenses.
- Scleral lenses are particularly helpful in the case of very irregular corneal shapes, such as the ones that are frequently found in advanced keratoconus. Instead of sitting on the cornea itself, as normal contact lenses do, scleral lenses sit on the sclera (the white part of the eye) and dome over the cornea without touching it at all.
FAQs
Who is affected by keratoconus?
Men and women can both be affected by KC. Symptoms typically show up in teenage years through early 20s.
What causes keratoconus?
While the cause of KC is undetermined, genetic and environmental factors are considerations. Many patients that present with keratoconus also have a parent that was diagnosed. Chronic eye inflammations from allergies or irritants and frequent eye rubbing may play a part in exacerbating the condition.
Can keratoconus occur only in one eye?
Yes. While keratoconus normally presents bilaterally, unilateral presentations are quite common.
Can keratoconus be prevented?
Most cases are not preventable. You may be able to reduce your chances of developing KC with good eye health and hygiene practices, like protecting your eyes from UV radiation, ensuring that contact lenses fit correctly, treating eye discomfort, and not rubbing your eyes.
I think I might have KC. What are my next steps?
If you are experiencing common symptoms of keratoconus, reach out to your eye doctor immediately to confirm diagnosis and start treatment. Early intervention is crucial to manage the progressive disease.
What are possible complications of keratoconus?
In addition to vision degradation, loss of vision, light sensitivity, and other symptoms listed in earlier paragraphs, KC can, in rare cases, cause a complication called corneal hydrops. This involves a breaking of the cornea, causing the fluid in the eye to flow abnormally into the cornea. This will cause severe pain, swelling, and, in some cases, sudden vision loss.
Is keratoconus always degenerative?
Keratoconus is a disease with a high degree of variability and unpredictability. While many patients have a mild form with a low degree of progression, there is not a good way to predict results. It is widely though that the incidence of KC is actually much higher in the general population, but it goes undetected due to very mild and non-progressive cases,
Keratoconus Treatment at Swagel Wootton Eye Institute
Swagel Wootton Eye Institute is one of the premier practices in Arizona. The practice has many experienced eye doctors on staff, including Dr. Renée Hanson, who specializes in treating keratoconus. Dr. Hanson previously practiced in Berkeley, CA, alongside a team of corneal specialists and managed keratoconus cases, corneal transplant cases, and pediatric ocular trauma cases for 15 years before joining SWEI. They use the latest technology to fit custom contact lenses, including the Visionary optics SMap profilometer. This technology allows Dr. Hanson to compile a virtual 3D mold of the surface of the eye in order to create a unique custom lens for almost any eye. This technology has greatly improved the accuracy and speed of a custom contact lens fit. Keratoconus is a serious condition and requires proper treatment to preserve and correct vision.
Dr. Hanson and the team at SWEI have a wealth of experience in dealing with KC cases and are ready to help patients achieve their best results. The state-of-the-art center has advanced diagnostic and surgical options to optimize patient outcomes.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]