Can You Prevent Keratoconus?

Scientists are still searching for a cause of keratoconus, a progressive eye disorder that diminishes eyesight. Fortunately, there are a few treatment options patients can consider to help keep their eyesight intact.
Keratoconus is a progressive eye disease that typically appears when a person is in their teens. Our eye doctors suggest scheduling an eye exam appointment early on to take the right preventative steps.
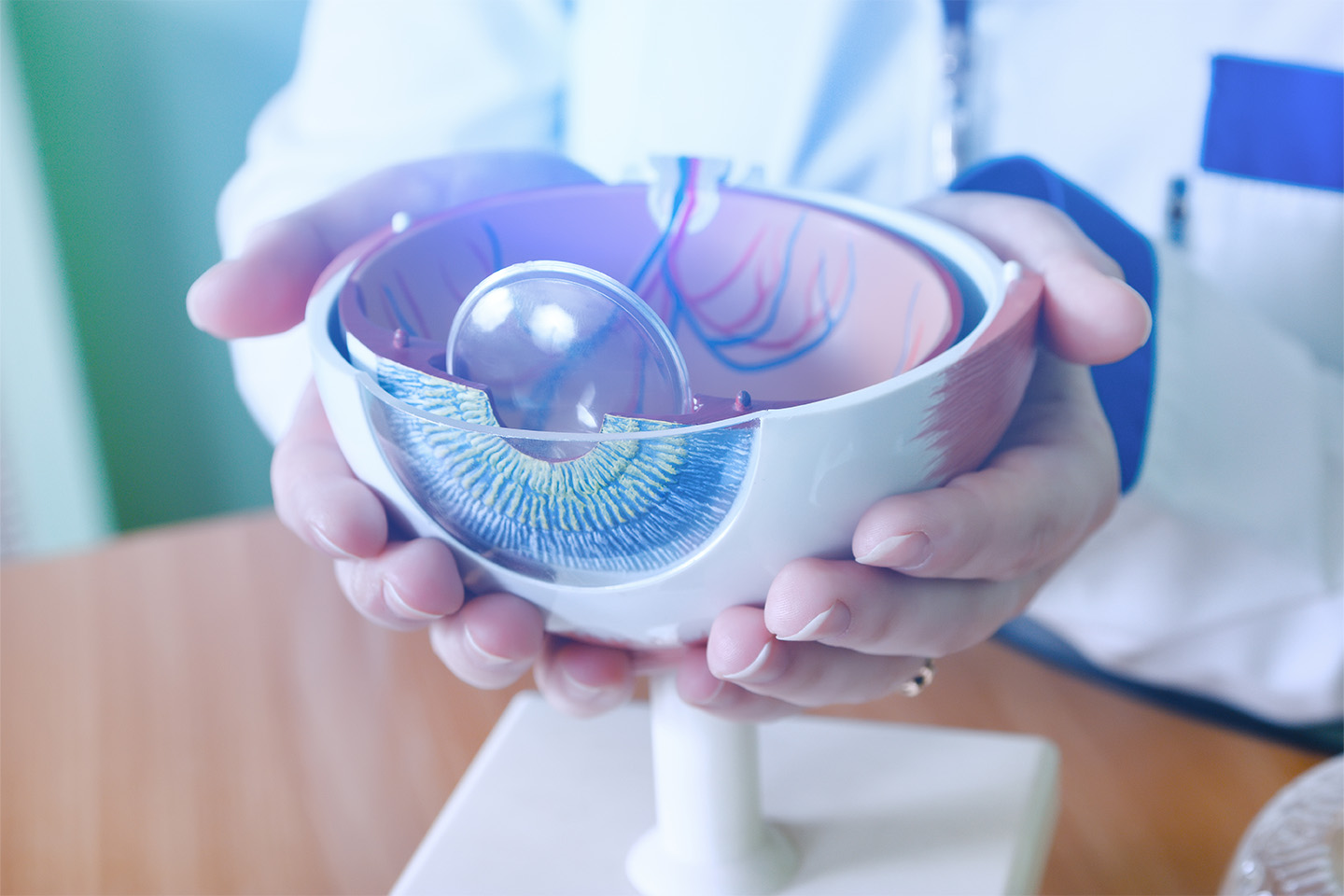
A normal cornea has a rounded surface that allows light to pass through it, traveling from the cornea to the brain and allowing us to see. But in corneas affected by keratoconus, the cornea becomes thinner and bulges out in an abnormal cone shape.
When the structure of the cornea changes, the cornea cannot properly convey images to the brain. As a result, keratoconus may cause nearsightedness, astigmatism, blurred vision, or double vision. It typically begins in one eye and then develops in the other.
A definitive cause has yet to be determined for the disorder, although genetics is a major factor. Other influences associated with the development of keratoconus include a breakdown in the corneal tissue, as well as environmental components such as UV exposure.
What Causes Keratoconus?
Since keratoconus runs in families, researchers have focused on genetics as the primary cause of the disorder. Recently, the National Eye Institute gave a $2.1 million grant to the Medical College of Georgia to further study whether mutations in the PPIP5K2 gene contribute to the onset of keratoconus.
Keratoconus has also been linked to an increase in oxidant stress in the eye. Normally, antioxidants clear away harmful substances and debris from the eye. In individuals with keratoconus, however, the amount of antioxidants to fight harmful substances decreases, leading to a weakening of the collagen in the corneal tissue. As the collagen thins out, it cannot hold the rounded shape of the cornea and instead it forms into a cone configuration.
Prolonged exposure to UV rays is also considered a contributing factor. People with keratoconus tend to rub their eyes excessively, but it’s not known whether excessive eye rubbing is a cause of the disease or a symptom. Those with keratoconus may rub their eyes in an effort to alleviate any discomfort the condition causes, especially in its early stages.
Due to the genetic component, children in families with the disorder should have their eyes checked beginning at age ten. An eye specialist will measure the shape of the cornea to determine if there have been any changes. If keratoconus is diagnosed, patients are advised to avoid rubbing their eyes and consider a number of treatments to correct their eyesight.
According to the National Keratoconus Foundation, the condition affects one in every 2,000 individuals. However, the organization notes that because many keratoconus cases go undiagnosed, the number may be higher in reality.
Keratoconus Treatments
As researchers search for a cause that may provide guidance on prevention, keratoconus patients can explore several options that lessen the symptoms and improve vision. Eyeglasses, for example, can correct mild cases of keratoconus. In addition, patients can be fitted with customized soft contact lenses or gas-permeable contact lenses.
Other therapies are available if new eyeglasses or contact lenses fail to give patients clearer eyesight. The following three treatments for keratoconus are typically among the recommended options:
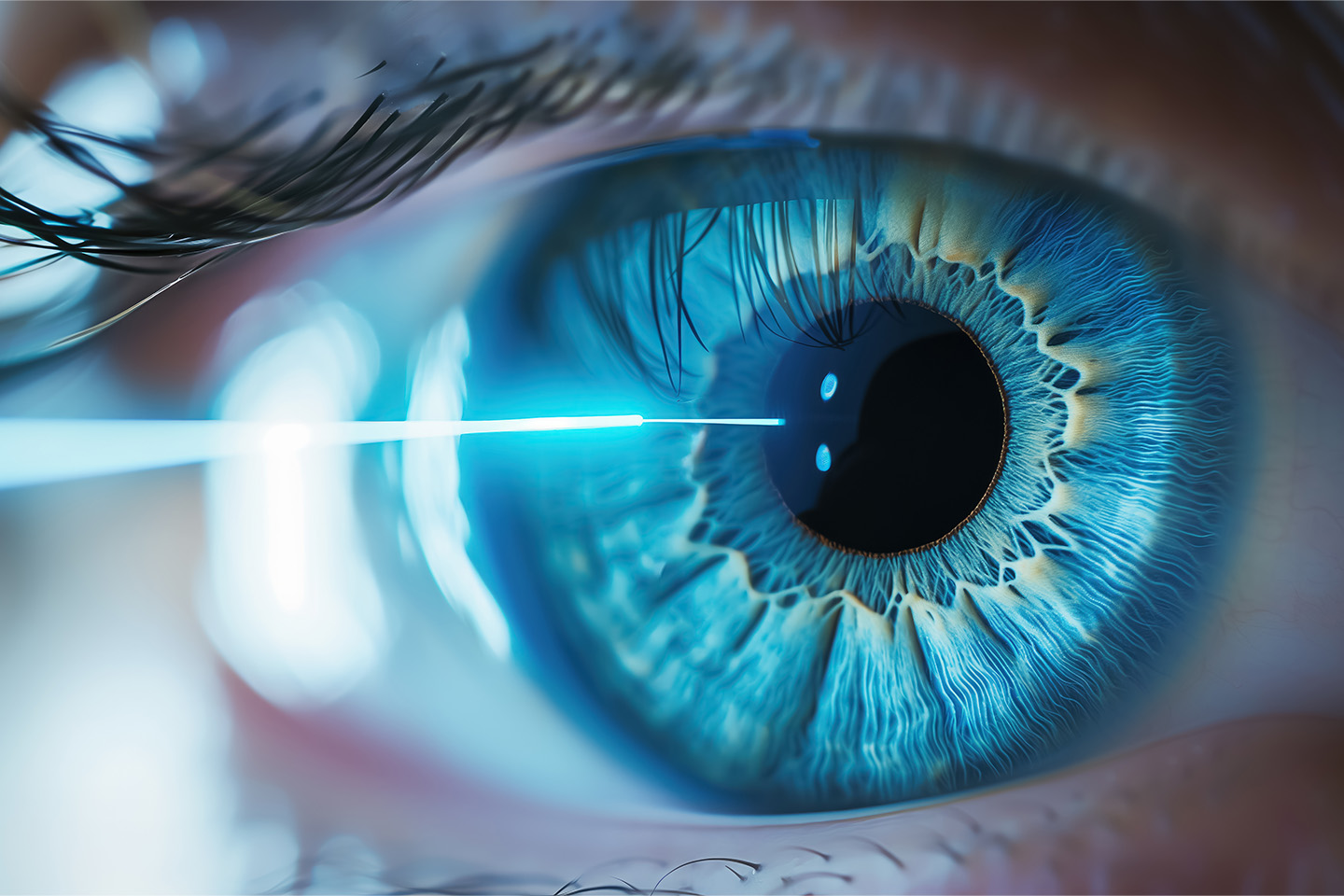
Corneal Cross-linking. To strengthen the corneal tissues and prevent the cornea from curving into a cone, riboflavin is injected into the cornea through the epithelium, or the outer layer of the cornea. In this procedure, the epithelium layer is either removed or left intact. Corneal cross-linking may reduce the need for corneal transplants in keratoconus patients further down the line.
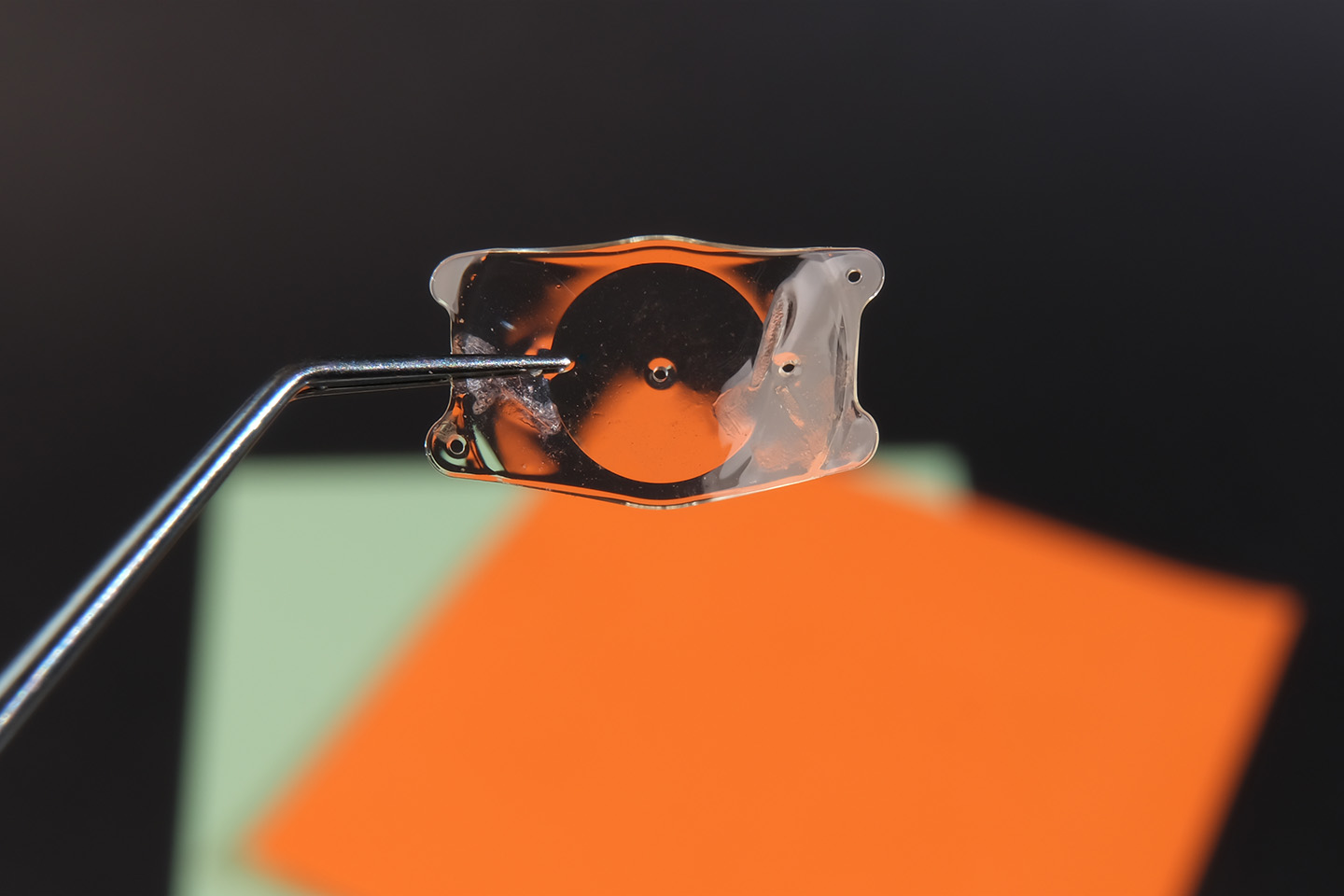
Intacs. Sometimes performed in conjunction with corneal cross-linking, arc-shaped Intacs are implanted in the cornea to improve its shape and consequently give patients clearer vision. This surgical procedure takes about ten minutes and is recommended for those whose vision hasn’t been improved with eyeglasses or contact lenses. Undergoing an Intacs surgery may not preclude patients from needing a corneal transplant if the disease continues to progress.
Corneal Transplant. If eyeglasses and customized contact lenses fail to upgrade visual acuity, patients may require a corneal transplant. After the center of the cornea is removed, a donor cornea takes its place.
Helping Patients Achieve Clearer Vision
At Swagel Wootton Eye Institute, our doctors can diagnosis keratoconus with a thorough eye exam and discuss treatment options with you. Your eyesight is important to us — if you believe you may be living with keratoconus or an undiagnosed eye condition, make an appointment with us today at our Mesa and Chandler locations.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]