Corneal Transplants: What Patients Need to Know

With a success rate of 90 percent for good candidates, corneal transplant surgery is a highly-effective way for patients with damaged corneas to improve their vision.
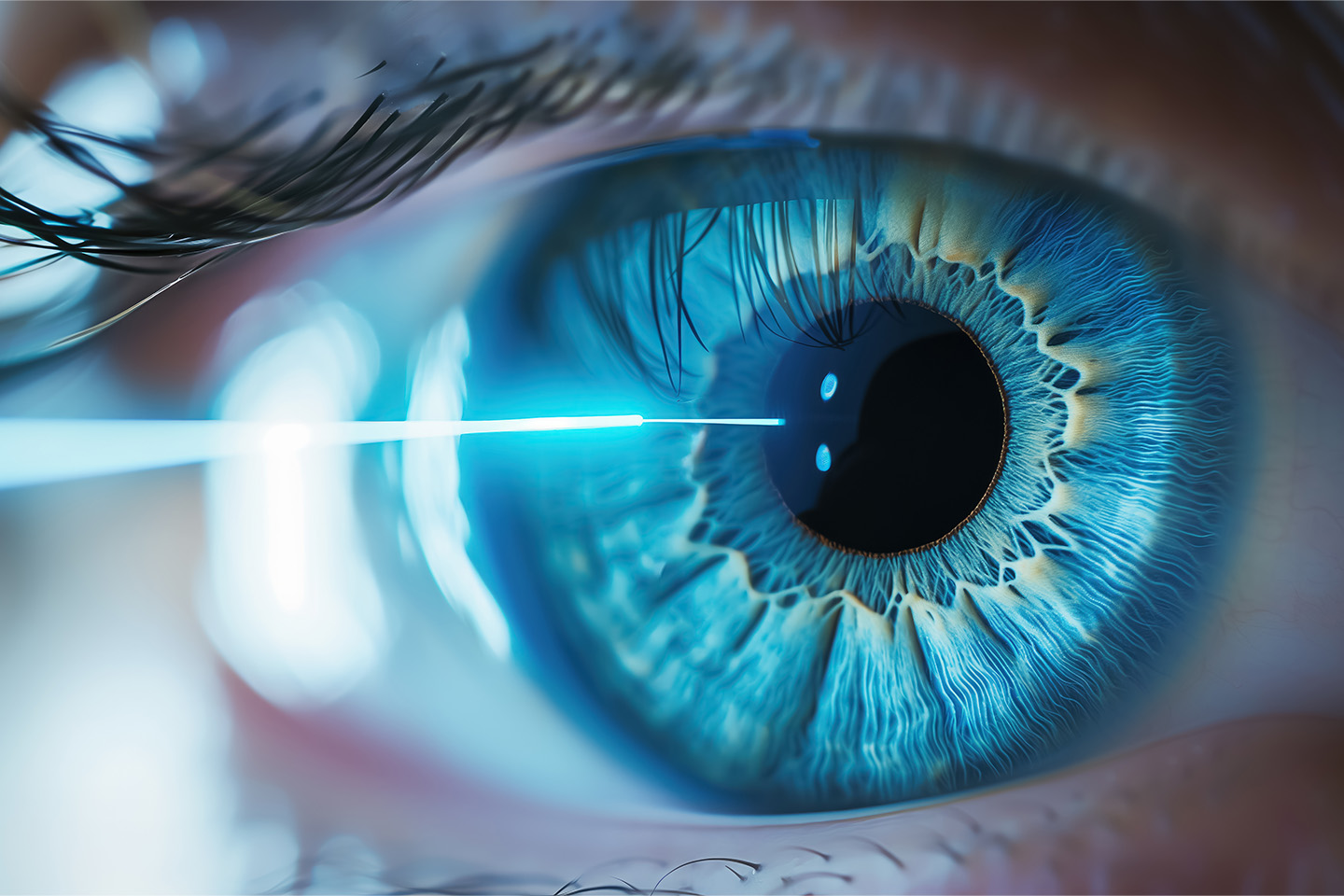
Do you have blurry vision or high sensitivity to glare? The issue might be your cornea, the clear front-most part of the eye that covers the iris and pupil. In circumstances where a corneal issue cannot be easily repaired, you and your doctor might determine that a keratoplasty (or “corneal transplant”) would be the most effective way to treat your damaged or infected cornea.
Below, we explore the most important things patients should expect before, during, and after a corneal transplant.
When Is a Corneal Transplant Appropriate?
A patient’s need to undergo a keratoplasty can stem from a wide variety of issues, including corneal scarring caused by infection, scarring caused by conditions like trichiasis (an inward turn of the eyelashes that scratches the cornea), bulging or swelling of the eye, genetic conditions like Fuchs’ dystrophy, and complications from previous eye surgery.
If you notice any of these symptoms, you and your doctor should discuss whether a corneal transplant may be right for you. The quality of your candidacy for a keratoplasty will depend on whether your vision plan covers the entire procedure, whether you can take the requisite time to acclimate to your new cornea after the operation, the effectiveness of less-invasive options like corrective eyewear, and the extent of the vision impairment and pain caused by your corneal issues.
What to Expect Before A Corneal Transplant
Once you’ve decided to have the procedure, you will receive a thorough eye exam from your ophthalmologist, during which your eye will be carefully measured for the new cornea. Underlying eye conditions like infection or inflammation will need to be treated before the operation can take place. Tell your doctor about all medications you are currently taking; you may have to pause taking medications like blood thinners.
You will then be placed on your local eye bank’s list of patients who are awaiting donor corneas. Corneas are donated much more frequently than other organs, so patients usually wait a few weeks at most.
Corneal transplants are almost always performed under local anesthesia. You will be awake, but you will feel little to no pain or discomfort. Your doctor may also administer anti-anxiety medication to keep you as relaxed as possible during the operation.
Types of Corneal Transplants
There are several kinds of corneal transplants. The kind you receive will depend on what part and how much of your cornea is damaged, and which procedure is likely to result in the best outcome.
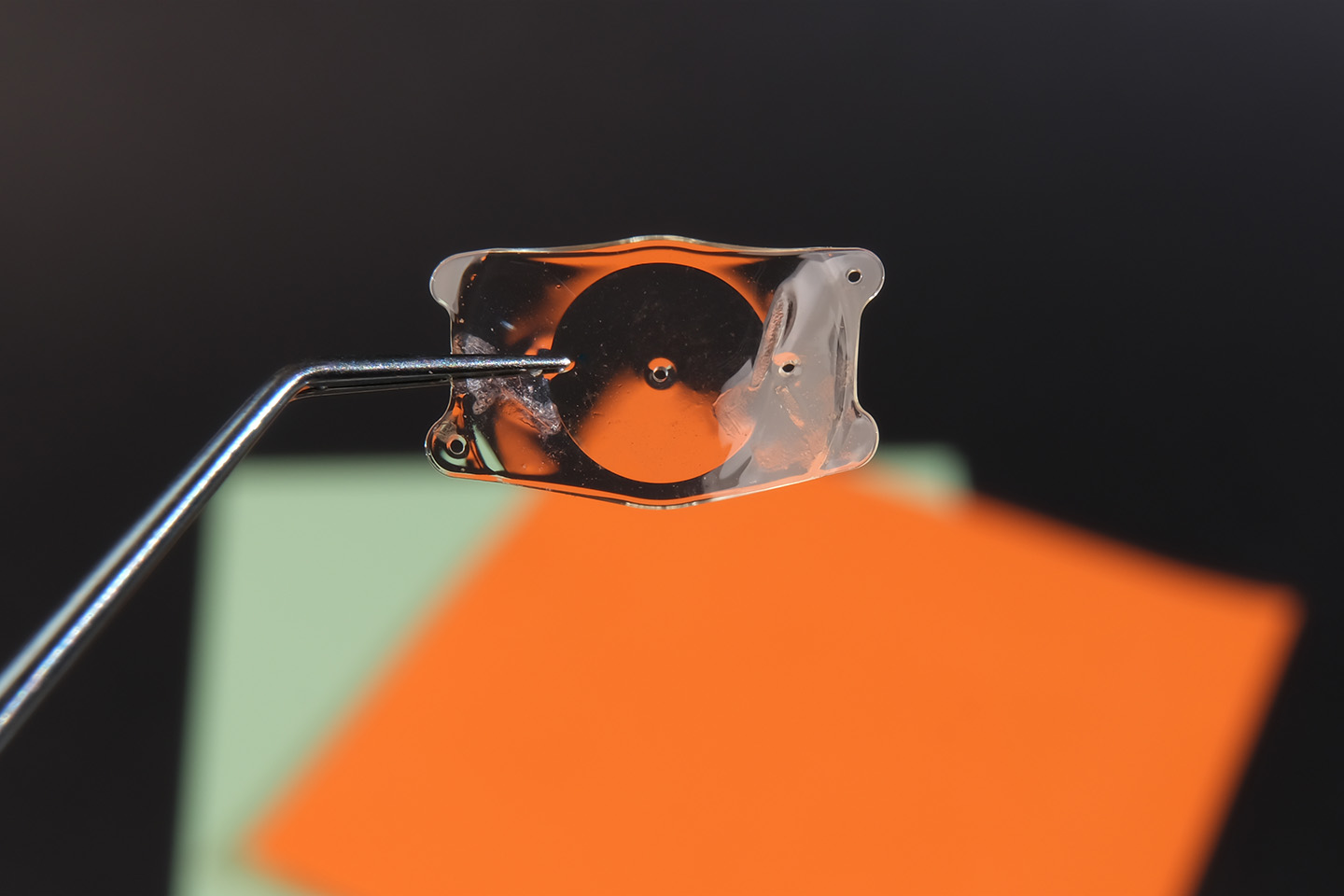
In a traditional full-thickness transplant, or penetrating keratoplasty, a disc of the cornea is removed using either a cookiecutter-like apparatus called a trephine or a laser instrument. The donor cornea is cut to size and sutured in place.
In an endothelial keratoplasty, only a thin layer of tissue is removed from the back of the cornea. The donor tissue is then implanted and positioned using an air bubble. Conversely, in an anterior lamellar keratoplasty, a thin layer of tissue is removed from the front of the cornea, meaning sometimes, sutures are not required for this procedure.
After Your Corneal Transplant
You will still be feeling the effects of the anesthetic for some time following the operation, so you will need to arrange for a ride home from your keratoplasty. Corneal transplants are usually outpatient procedures, allowing you to resume a relatively normal lifestyle in just a day or two.
That said, it can take several weeks for your vision to stabilize after a corneal transplant, and it can take up to a year for your eyes to recover fully. In the days following your procedure, you should protect your eyes by wearing an eye shield — especially at night — and be careful when performing strenuous activities. You should also schedule regular follow-up appointments with your ophthalmologist to keep tabs on how your eyes are healing.
In one out of ten cases, the body’s immune system will attack the donated cornea, a reaction known as “corneal rejection.” If you are experiencing pain, poor vision, sensitivity to light, or redness, contact your ophthalmologist immediately, as these may be signs of corneal rejection. Doctors can treat corneal rejection by prescribing medication or performing a new transplant.
If you or a loved one is experiencing pain or swelling in the eye, consider reaching out to the specialists at Swagel Wootton Eye Institute. We have the experience and expertise to determine if a corneal transplant is right for you. Contact us at our Mesa and Chandler locations today for a consultation.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]