How Diabetes Impacts Eye Health: Conditions and Prevention Tips

According to the Centers for Disease Control and Prevention, approximately 38 million adults in the U.S. have diabetes. This condition impacts how your body regulates blood sugar through the release of insulin and can have far-reaching effects on your health, including your heart, kidneys, and skin. Diabetes can also affect your eye health, causing vision loss and blindness. Diabetic eye disease is a group of eye conditions that can affect people with type 1 diabetes, type 2 diabetes, or gestational diabetes. Here’s how diabetes can affect your eyes, the conditions it can lead to, and the steps you can take to protect your vision.
The Connection Between Diabetes and Eye Health
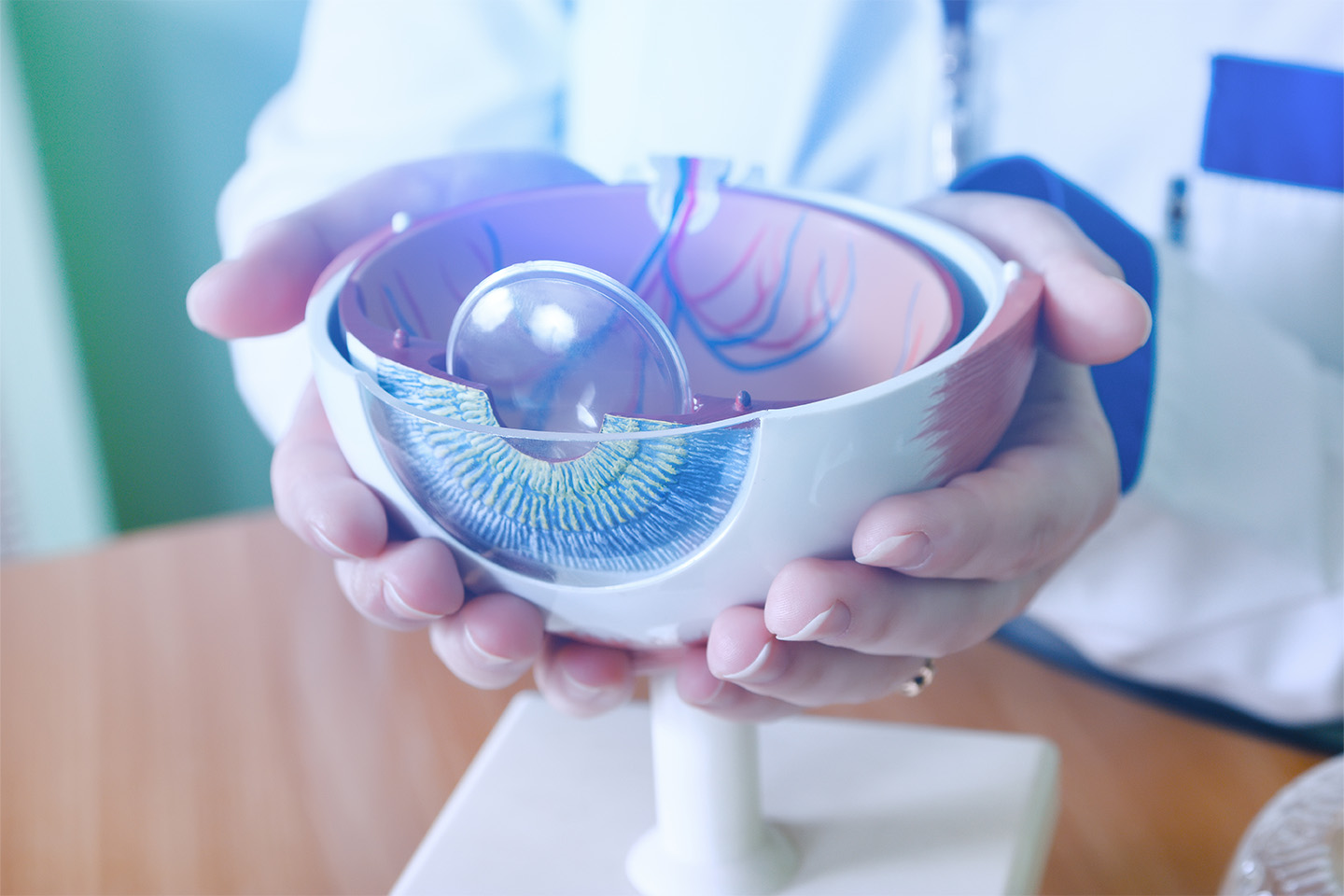
When your body stops responding to insulin, too much sugar can remain in your blood and cause high blood sugar levels (blood glucose). The excess sugar can lead to blockage of the blood vessels and stop blood flow, damaging the blood vessels. This damage can happen to the tiny blood vessels in the retina, the layer of light-sensitive tissue at the back of your eye. High blood sugar is not likely to cause long-term vision loss if corrected right away, but people with diabetes who are changing medications or diabetic care plans may experience temporary blurred vision until glucose levels return to normal. Over time, though, the damage — which can begin during prediabetes when blood sugar levels are elevated but not yet high enough to be diagnosed as diabetes — can lead to a range of other eye problems that can compromise your vision.
Types of Diabetic Eye Disease
There are four main eye conditions linked to diabetes that can threaten your sight.
Diabetic Retinopathy
Diabetic retinopathy is the most common cause of vision loss for people with diabetes. The risk for this condition increases the longer you have diabetes and the longer your blood sugar remains unmanaged. There are two main stages of diabetic retinopathy:
- Non-proliferative diabetic retinopathy (NPDR): In this early and most common stage of diabetic retinopathy, blood vessels in the retina stop growing, or proliferating, and their walls become weakened. This may cause the blood vessels to swell and leak fluid and blood into the retina. Symptoms typically aren’t noticeable during this stage, but individuals may experience changes that may come and go to their vision, such as difficulty reading or seeing objects at a distance.
- Proliferative diabetic retinopathy (PDR): During this advanced, more severe stage, new, fragile blood vessels grow in the retina after the damaged vessels close off. These new vessels can leak into the eye’s vitreous humor, the clear gel-like substance that fills the space between the eye’s lens and retina, causing severe vision loss or blindness. Symptoms can include blurry vision, white or translucent vision blockers (floaters), faded colors, and blank or dark areas in your field of vision.
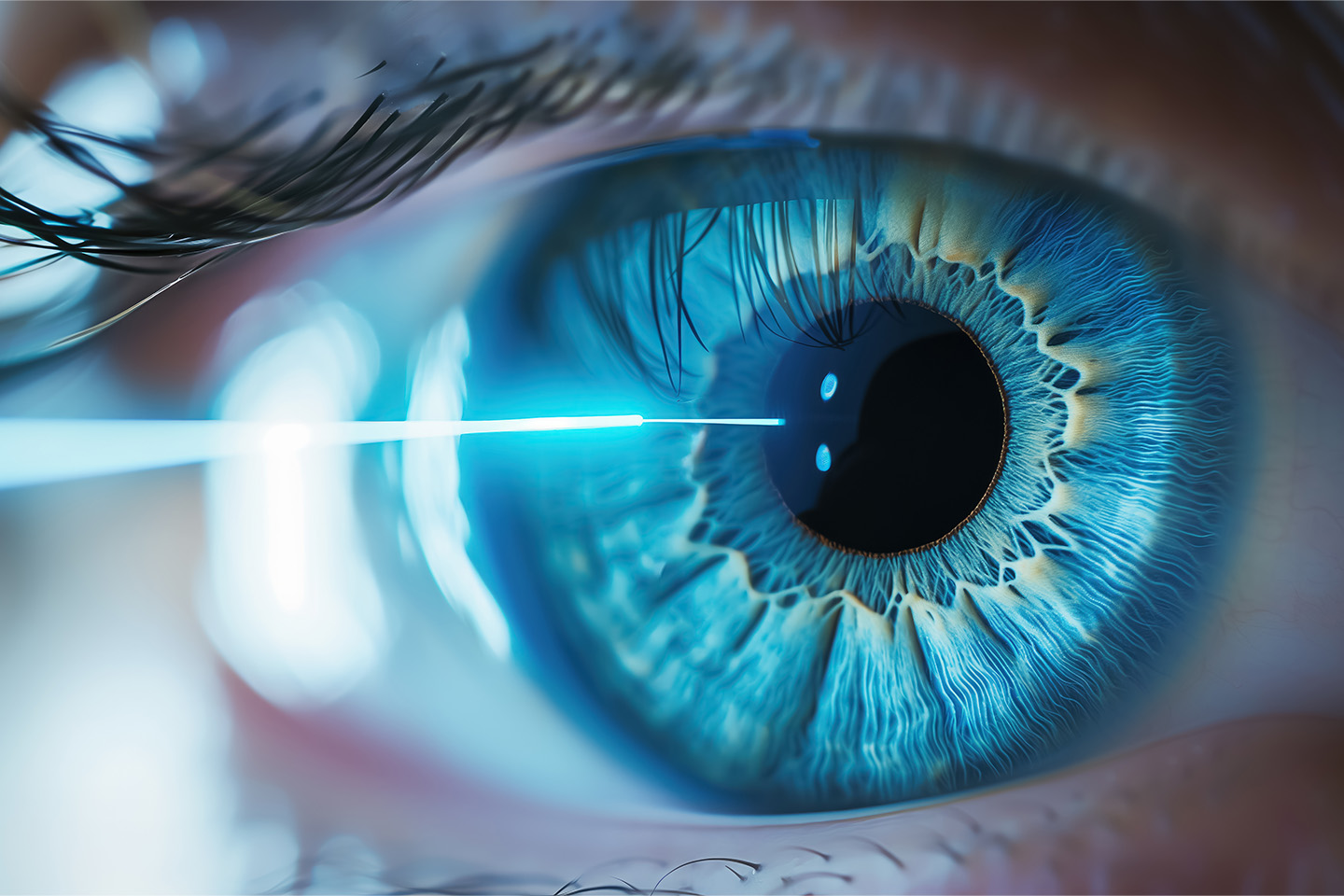
Treatment for diabetic retinopathy will not reverse vision loss, but it can prevent further damage. Treatment options can include injections, such as anti-vascular endothelial growth factor (anti-VEGF) and corticosteroids; laser treatment to shrink the blood vessels and reduce swelling; or an eye surgery called vitrectomy.
Retinal Detachment
Retinal detachment can be a complication of diabetic retinopathy. Scar tissue from the growth of new blood vessels can eventually cause the retina to separate from the back of the eye. When this occurs, you may notice flashes of light, floaters, or severe vision loss. Retinal detachment should be treated as a medical emergency to prevent further risk of permanent vision loss.
Diabetic Macular Edema
Left untreated, diabetic retinopathy can develop into diabetic macular edema (DME). DME occurs when fluid leaks into the macula, the part of the retina responsible for sharp, central vision. This leakage causes the macula to swell, leading to blurred or distorted vision. DME can occur at any stage of diabetic retinopathy and affects approximately 1 in 15 people with diabetes. Treatments for DME are the same as those for diabetic retinopathy.
Glaucoma
Diabetes increases the risk of developing certain types of glaucoma, including open-angle glaucoma and neovascular glaucoma. The growth of new blood vessels can block fluid from properly draining from the eye, leading to increased intraocular pressure (IOP) and damage to the optic nerve. If not treated early, glaucoma can lead to irreversible vision loss and blindness. Treatment depends on the type and severity of the condition and may include eye drops, oral medication, laser treatment, or surgery.
Cataracts
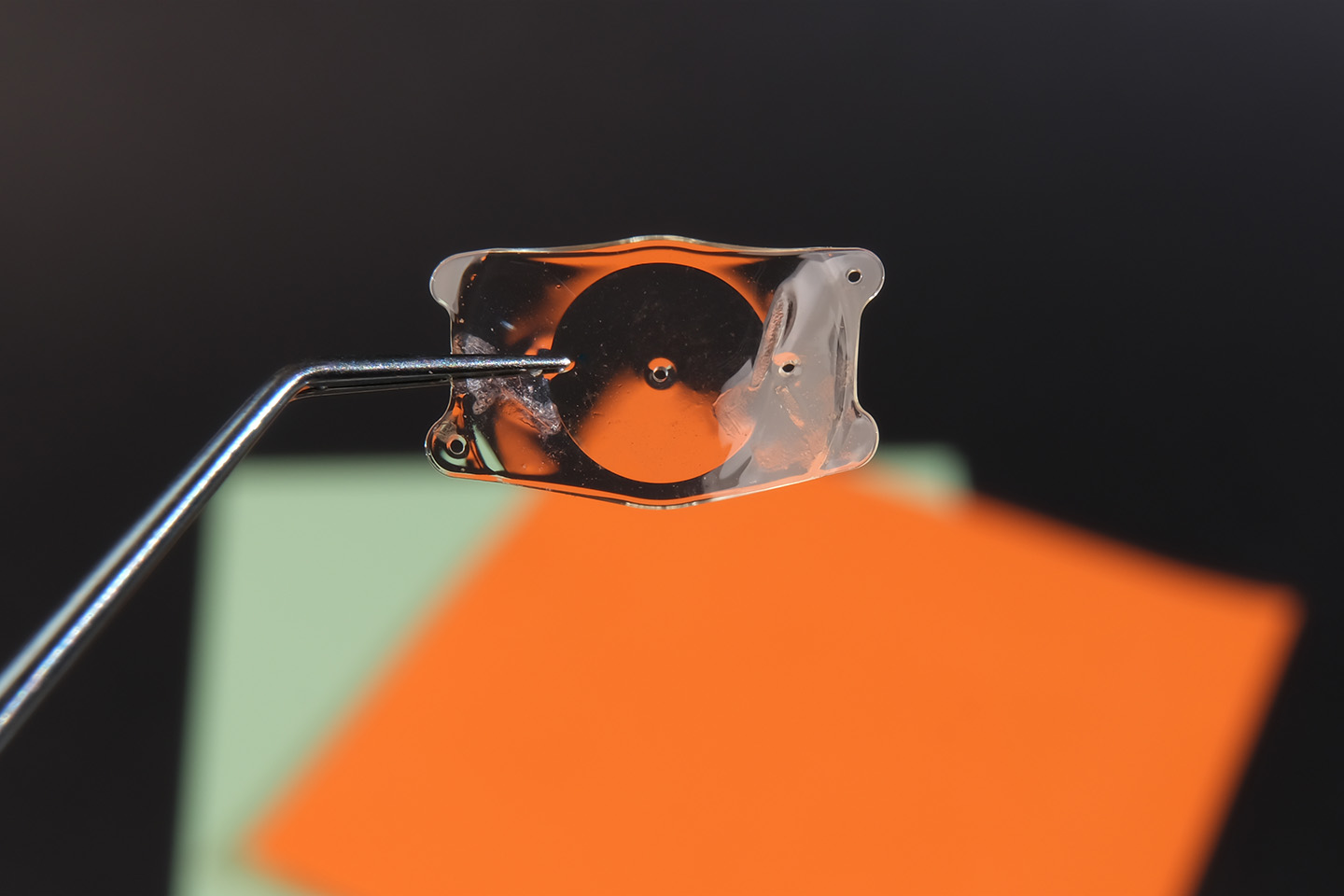
People with diabetes are two to five times more likely to develop cataracts than those without diabetes and are at a higher risk of doing so at an earlier age. High blood sugar can cause structural changes to the eye’s lens, making it more susceptible to accelerated cataract development. Cataract symptoms often progress over time and can include cloudy or blurry vision, yellowing or fading of colors, double vision, and light sensitivity. Cataract surgery is a common and effective way to restore your vision.
How to Prevent Diabetic Eye Disease
Managing diabetes effectively is crucial in lowering your risk for diabetic eye disease. Here are some steps you can take:
- Monitor your blood sugar regularly and work with your care team to control your diabetes.
- Get regular physical activity, eat a nutritious diet, and take all insulin and other diabetes medications as instructed to help keep your blood sugar in a healthy range.
- Schedule regular comprehensive eye exams with dilation for early detection and management of diabetic eye conditions. Diabetic eye exams consist of the same tests as a comprehensive eye exam with a specific focus on the retina. They are designed to monitor and detect diabetes-related eye complications, including diabetic retinopathy. Talk to your eye care provider about how often you should schedule these exams for your unique health situation.
Committed to Your Eye Care
At Swagel Wootton Eye Institute, we prioritize protecting your vision and helping you see your best. For individuals with diabetes, following recommended eye exam schedules and informing their eye doctor about any vision or eye health changes is crucial. Contact us today to learn how we can help you prevent diabetic eye disease.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]